As Africa holds its first ever conference on clubfoot – something about one in 800 people across the world are born with – the BBC visits a health clinic in Senegal to witness a transformative treatment which is turning lives around.


Earlier this year, 14-year-old Serigne was reluctant to ever leave the house. He could walk very slowly, but – born with both his feet pointing inwards – he was just too ashamed. Some would make fun of the way he walked, others were afraid and would call him names. But now, less than six months on, his feet are transformed and his dream of playing football for Senegal seems at least possible.
Serigne has clubfoot, also known as talipes, and today is another step in the journey to correct that.
According to the charity MiracleFeet, of the nearly 10 million people alive today who were born with clubfoot, as many as eight million have never received treatment. Senegal has been a relatively late adopter of Ponseti – a pioneering method of correcting clubfoot named after the Spanish doctor who invented it – compared with some other African countries. Malawi and Uganda, for example, were ahead of many Western countries in recognising its potential. But this means Senegalese medics have perfected the original concept and are now using it to treat teenagers or even adults who thought they had passed the age for any intervention.
Serigne’s mother is beaming at her son’s progress. She knows better than anyone the cruel nature of this disability.
“One time he even refused to leave home for three days. It caused me so much hurt inside. But now we’re happy.”




As part of the Ponseti method, a new plaster cast is put on every week to gradually manipulate the foot into a better position. Because his case is so severe, he has had 20 casts in as many weeks, but the average is between five and eight. As with most cases, towards the end of his treatment a minor operation to release his Achilles tendon has been required, but otherwise this treatment is non-invasive.
Better still, it is low cost, doesn’t need to be done by highly-trained surgeons, and is extremely effective – 90% of children receiving help under the age of two with routine cases will be left with good foot function, whereas surgery can lead to complications. The change is truly astonishing when you look at the video footage of Serigne’s shuffle before treatment began.
A few days ago, Serigne had his final cast put on. After that, he will need some physiotherapy to help him learn to bear weight on his legs, and he must initially wear short leg braces to keep his feet in position, but his future is very promising.
Fatou, another child being treated in this Dakar clinic, has travelled 400 miles (644km) to get the same treatment for her right foot. Today is her 13th birthday but the day is starting with the removal of her fourth cast. The nurses saw through the plaster and then, in a cloud of dust, prise it off her leg. She winces a little, but the clinic’s head nurse, Nicanor Manga, reassures her that some pain is normal and it will be worth it in the end.
“We believe that her foot will be corrected and that later on she will be able to walk properly,” he says. “Really, it’s a joy for us,” he smiles. “When we lift the cast off and see the good progress, we’re really happy.”


Fatou explains that because she lives in such a remote part of the country, she never expected to get her foot corrected. So she is happy to be patient.
School has been hard – watching other children run around and jump – whereas Fatou has been forced to rely on crutches.
“Everything I longed to do, I couldn’t. But once I’m cured, I’ll be able to do anything I want.”
That includes working towards achieving her new dream of becoming a doctor, so positive has been her experience here.
But not everyone is so fortunate. Take 32 year-old Oumou Barry, for example. When we visit her in Lac Rose, a suburb of the Senegalese capital, she shows us her left foot, which is bulky and misshapen. She hobbles on the side of her foot and shooting pain means she can’t walk far. Her life has been marked by the stigma of clubfoot, and she wipes away tears as she recalls her childhood.
“I used to ask my mother why I was like this? She would answer me: ‘It’s God’s will’ and ‘You were born like this.'” Oumou has experienced exactly the kind of fatalism that stops many families in Senegal from seeking treatment.
She says her toughest time was during her teens, when her friends began wearing heels, but she had to stick to sandals. In the end she dropped out of school – no longer able to cope with the bullying.
Even away from spiteful classmates, life was tough. She had to give up on a sewing course when she discovered that operating the sewing machine pedal was just too painful.
Oumou has a husband and two children so her life isn’t as isolated as some who have been ostracised because of clubfoot, but she still feels the limitations of a very visible disability which has left her unemployed.
“I hold on to nothing concrete,” she weeps.
Unfortunately, due to her age and a botched surgery, Oumou is not able to receive Ponseti treatment. Some adults can respond well to Ponseti, but it is more complicated because their feet are less supple.
In most cases, the exact causes of congenital clubfoot are still not well understood, although boys are twice as likely than girls to be born with it. The vast majority of global cases are in low and middle income countries, due to high birth rates, and it’s in poorer countries that the condition is most likely to go uncorrected.
One woman who has dedicated her life to making sure fewer people reach adulthood with clubfoot is Aisha Mballo. When we meet her, she is walking confidently through a market in the town of Thies, a big picture book under her arm. The book explains clubfoot and how the Ponseti method can correct it. She has come here to seek out cases of clubfoot which might otherwise go undetected.
Aisha says her own feet were “completely turned backwards” until, in the 1990s when she was in her mid-teens, she was sent to the US for complex surgery. Now she volunteers as an ambassador for the charity MiracleFeet, championing early screening for newborns.
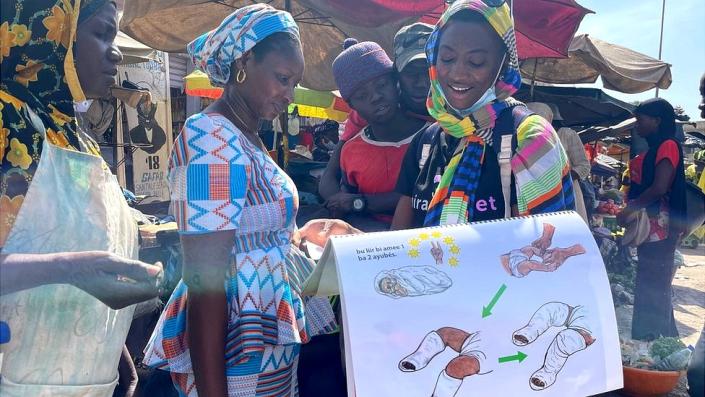
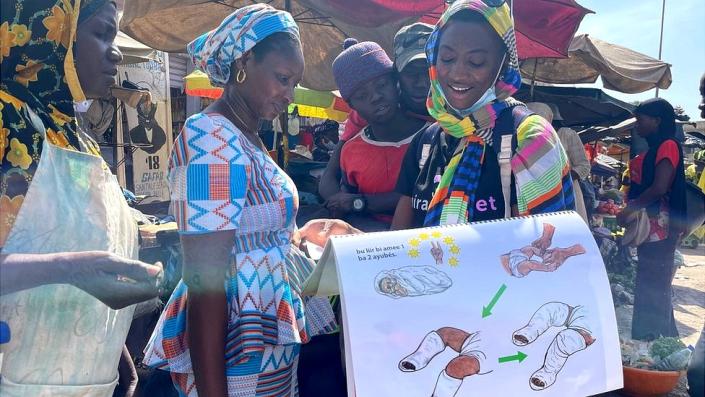
“If people recognise the condition and get their kids out of hiding, we can get them to hospital for treatment.”
Rosalind Owen of the Global Clubfoot Initiative, who has studied the perception of clubfoot in Africa, says that in traditional communities there are “huge problems with stigma”.
“People think you were cursed, or had witchcraft against you, or perhaps that your parents did wrong.” This can include, she says, a belief that the mother committed adultery and this is the punishment.
Still, fewer than 20% of clubfoot cases are receiving treatment at birth in Senegal, so there’s a lot of room for improvement.
Before leaving Thies, we drop in on another clinic to see a two-week-old baby girl getting a new plaster cast.
The doctors and nurses are winding bandages around her tiny legs and then smoothing down wet plaster on top.
This is the ideal time to correct clubfoot.
In the waiting room, a two-year-old boy, possibly a budding footballer, is kicking a juice carton around. He’s a little unsteady – with one foot still turned inward – but at least he’s getting the treatment he needs.
Photography and additional reporting by Gabriella O’Donnell and Nick Loomis