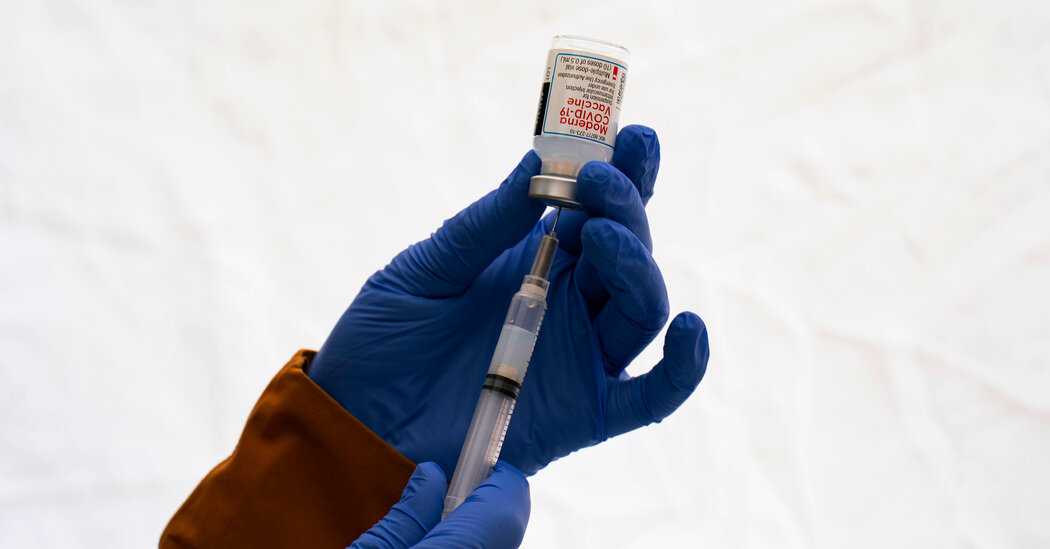
Moderna announced preliminary results Tuesday from its study of a coronavirus vaccine intended to protect against variants, saying the findings show it can design a vaccine that offers better, longer-lasting protection than its initial product.
But the company said it was also testing another version of the vaccine that it expected would do even better, with results expected in late May or early June.
The company’s findings, published in a paper without being evaluated by outside scientists, offer hope that the nation will have a better vaccine by the fall, when the coronavirus is considered likely to re-emerge in force.
Researchers at Moderna, other pharmaceutical companies and the National Institutes of Health have been racing to figure out how to redesign the existing vaccines in time for new booster doses to be manufactured over the summer. Moderna’s results are the first of their kind to be released.
The vaccines from Moderna and Pfizer-BioNTech continue to strongly protect most people from hospitalization and death caused by Covid-19. But their potency against infection wanes quickly. Federal officials recently authorized additional shots for people 50 and older, citing concerns about waning protection against severe disease in vulnerable populations.
Moderna said its research showed the promise of a so-called bivalent vaccine, even against other variants besides the two versions of the virus specifically targeted. In this case, researchers combined the existing vaccine with one designed to attack the Beta variant, which was first detected in late 2020. They found the combination provided a stronger defense not only against those forms of the virus, but also against the Delta and Omicron variants, the company said.
Volunteers who got a booster shot of the reconfigured vaccine produced more than two times the level of antibodies against the Omicron variant compared with those who got a booster dose of the existing Moderna vaccine. The added protection persisted for six months against the Omicron variant but fell against Delta to essentially the same level as that elicited by the existing vaccine, the study showed.
Moderna said although Beta was an early variant, it was relevant to test because it contains several mutations that “have been persistent in more recent variants of concern, including Omicron.”
Dr. Paul Burton, Moderna’s chief medical officer, said in an interview that he was betting on even better results from combining the existing vaccine with one aimed at Omicron. While the Beta variant faded months ago, Omicron is producing a stream of subvariants, including BA.1 and BA.2, and many experts suggest it is probably the best target for a new vaccine.
Given the ability of the Omicron variant to evolve, Dr. Burton said, “I think we have to just assume it is going to be major player, still, in the fall.”
Moderna’s researchers measured levels of antibodies — the body’s first line of defense in warding off infection from the coronavirus. Other immune responses that also defend against Covid-19 disease were not measured; those tests are far more complex and expensive to conduct.
But while antibody levels provide only a partial picture of the immune system’s responses, “we are still are thinking that keeping antibody levels high is important,” Dr. John Beigel, the clinical research director overseeing N.I.H. vaccine trials, said in a recent interview.
The sprint to update the vaccines involves small clinical trials paired with laboratory tests. First, vaccines are designed to target a variant — either alone or in combination with the original prototype of the virus or another variant.
A small group of volunteers receive the reconstituted vaccine. Then researchers at a laboratory test their blood samples for neutralizing antibodies against the whole array of variants — not just the one or two the vaccine was designed to attack.
Dr. Beigel said antibodies created by the coronavirus vaccine decayed at different rates, depending on the variant at play. “That is why we need six months’ worth” of data, ideally, to assess how well any updated vaccine would work, he said.
Some researchers suggest that a protein-based vaccine, perhaps like the one developed by the companies Sanofi and GSK, might prove to be a better booster than new versions of the Moderna or Pfizer-BioNTech vaccines used to vaccinate about 250 million Americans.
Dr. Burton said Moderna’s results on its Beta bivalent vaccine were “very reassuring” both in terms of safety and the immune response. But he said the company was eager for results by June from its bivalent vaccine aimed at the Omicron variant. Stéphane Bancel, Moderna’s chief executive, said that vaccine “remains our lead candidate” for a booster this fall.
If a bivalent vaccine that targets the Beta variant works well against Omicron, Dr. Burton said, one that targets Omicron itself would presumably work even better. He said he hopes the other study will show high and lasting levels of antibodies against both Delta and Omicron.
“That two months is worth waiting for,” he said. Ultimately, federal officials are aiming for a once-a-year booster shot.
Of about 900 volunteers in the Beta bivalent trial, one-third got a 50-microgram dose of the updated vaccine — the same dosage now authorized for a booster shot of the existing vaccine. The rest received a 100-microgram dose. The volunteers had fewer side effects from the weaker dose, and Dr. Burton said the company would probably settle on that dosage.
The study was not intended to evaluate vaccine effectiveness; it only measured the immune system’s response, which can point to efficacy.